Urinary Bladder Cancer

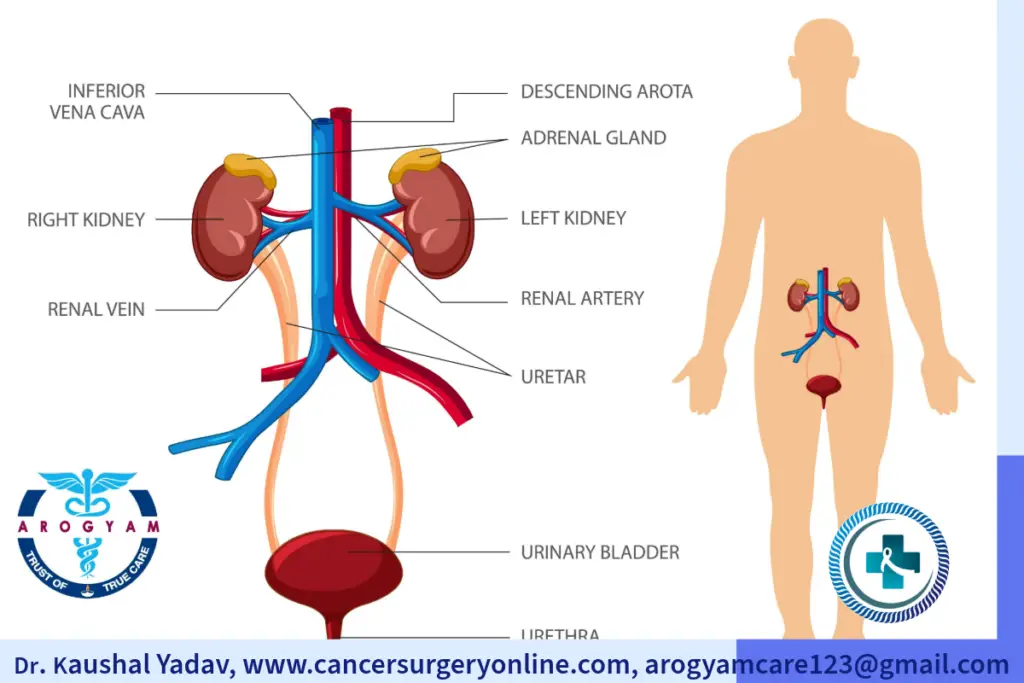
The urinary bladder is a part of our urinary system that stores urine before we urinate. It is a hollow, muscular organ that can stretch and shrink depending on how much urine it contains. The bladder is located in the lower abdomen, behind the pubic bone. It has four parts: the dome, the base, the body and the neck. The neck connects to the urethra, which is the tube that carries urine out of the body. Urine is produced in kidneys and through tubes called ureter it travels to urinary bladder. The bladder can hold about 500 to 700 mL of urine, but we usually feel the urge to urinate when it reaches about half of its capacity
Urinary bladder cancer is a type of cancer that starts in the cells that line the inside of the bladder.
Types
- Urothelial Carcinoma: 90% of urinary bladder cancers. Urothelial Carcinoma also occurs in renal pelvis, ureter and urethra.
- Squamous Cell Ca: 5%. This type is also associated with schistosoma haematobium infection.
- Adenocarcinoma: arise in the embryonal remnant of the urachus on or above the bladder dome.
- Undifferentiated
Risk Factors
 Age: More common beyond 50 years
Age: More common beyond 50 years- More common in males than females
- Tobacco: most common risk factor.Continued tobacco smoking is also associated with more disease recurrence and worse disease biology.
- Occupation exposures: paint, dye, metal, lether and petroleum industry.
- Environmental exposure: diesel engine exhaust, water contamination with arsenic
- Drugs like cyclophosphamide, pioglitazone
- Radiation exposure
- Chronic Irritation: infection with Schistosoma haematobium, chronic urinary catheters
- Genetic Cancer Syndromes: Lynch syndrome (hereditary non-polyposis colorectal cancer, or HNPCC)
* Avoiding smoking and protective measure at industrial exposure reduce 70% risk of urinary bladder cancer.
Screening for Colorectal Cancer:
- Screening not advised routinely.
- Industrial companies that use dyes, chemicals, and rubber products should explain the risks of prolonged exposure. Workers should be tested periodically with urinary cytology and urine routine examination. They should wear protective masks during working hours.
Alarmimg Signs and Symptoms of Urinary Bladder Cancer
Symptoms of Urinary Bladder cancer
Symptoms of Urinary Bladder cancer
Symptoms of Urinary Bladder cancer
Symptoms of Urinary Bladder cancer
Symptoms of Urinary Bladder cancer
Investigations for diagnosis of urinary bladder cancer
- Urinary tumor markers: Most commonly urinary cytology. It has low sensitivity.
- Cystoscopy: Flexible or rigid thin scope is inserted through urethra to check inside urinary bladder.
- CT urography: New Gold standard for urinary tract imaging for checking bladder tumor and synchronous tumors in other locations.
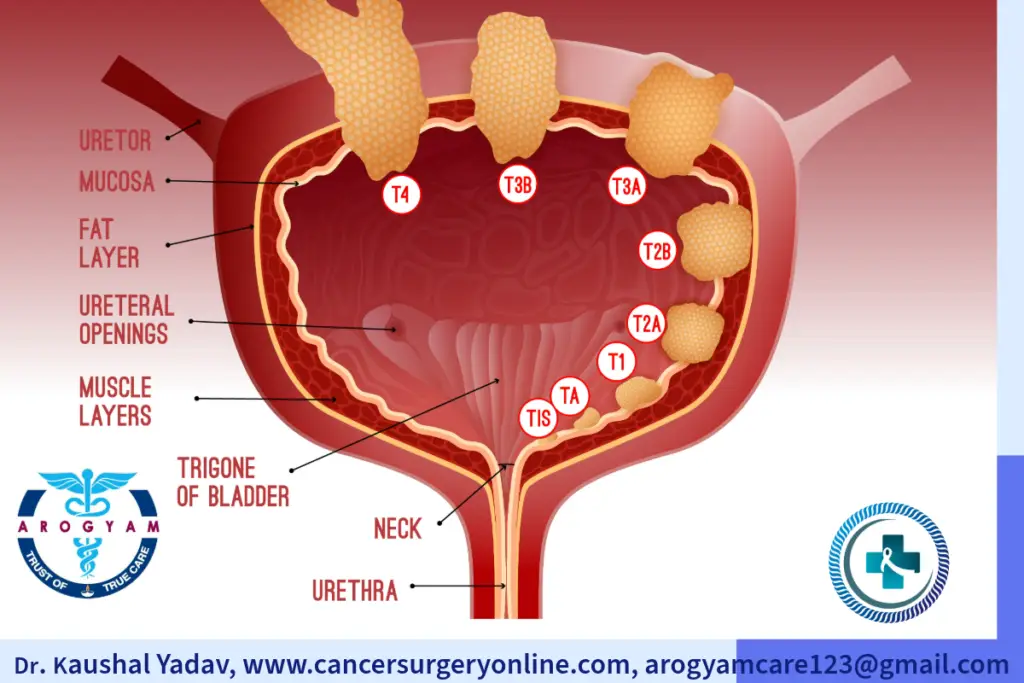
Stages of urinary bladder cancer are broadly classified into:
Cancer limited only to superficial layer of urinary bladder. Two third cases of bladder cancer are usually superficial.
Cancer spread inside deep muscle layer of urinary bladder but remain confined to urinary bladder.
Cancer spread beyound urinary bladder to other organs like liver, lung etc.
Treatment of Urinary Bladder Cancer
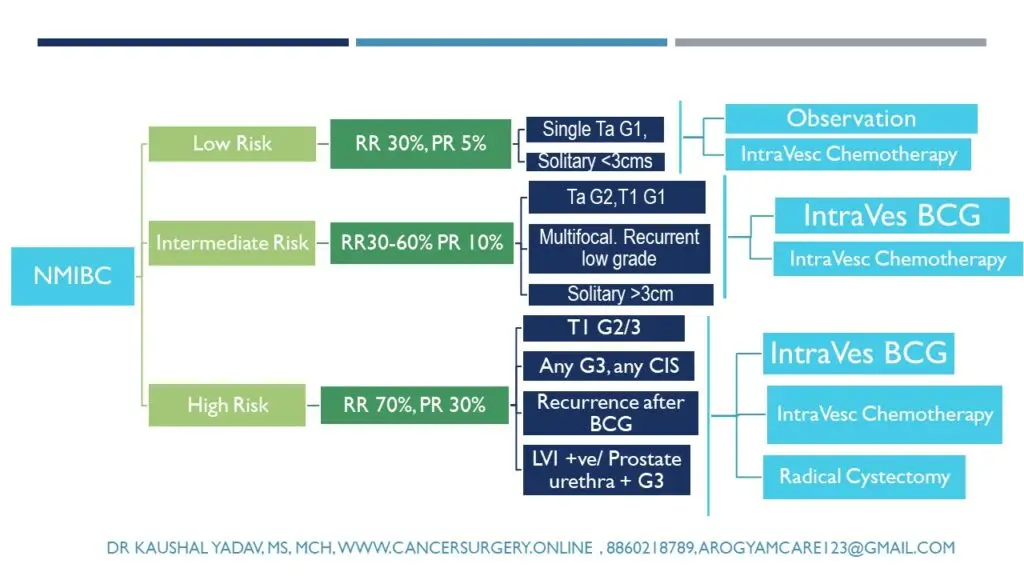
Non Muscle Invasive Bladder Cancer Treatment
Non muscle invasive bladder cancer is more common than muscle invasive bladder cancer, and it usually has a better prognosis. However, it can recur or progress to muscle invasive bladder cancer over time, so it requires careful monitoring and treatment.
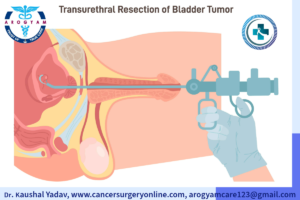
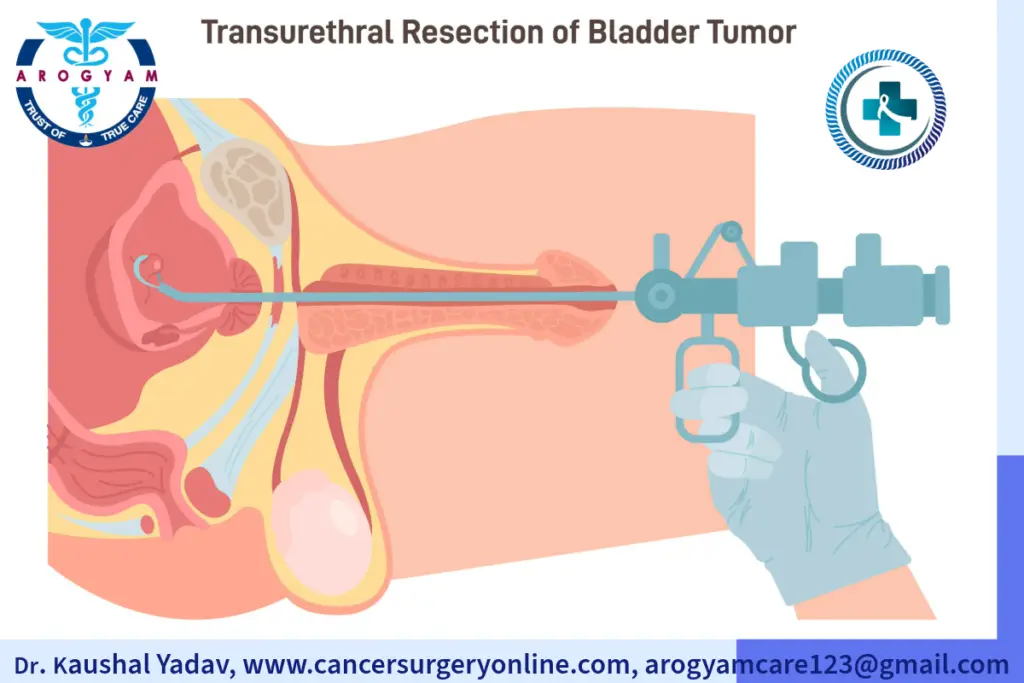
- Transurethral resection of bladder tumor (TURBT): This is a surgical procedure that involves inserting a thin tube called a cystoscope through the urethra into the bladder. The cystoscope has a small camera and a wire loop that can cut or burn away the tumor. TURBT is usually done under general or spinal anesthesia, and it can remove most or all of the visible tumor. TURBT is often the first treatment for non muscle invasive bladder cancer, and it may be repeated if new tumors appear.
- Intravesical therapy: This is a treatment that involves putting a drug in liquid directly into the bladder through a catheter. The drug can kill any remaining cancer cells or prevent them from growing back. Intravesical therapy is usually given after TURBT, and it can be either immunotherapy or chemotherapy.
- Immunotherapy uses drugs that stimulate the body’s immune system to fight the cancer, such as Bacillus Calmette-Guerin (BCG) or interferon.
- Chemotherapy uses drugs that kill or stop the growth of cancer cells, such as mitomycin C or gemcitabine.
Intravesical therapy is usually given once a week for six weeks, and then less often for maintenance.
- Cystectomy: This is a surgery that involves removing part or all of the bladder. Cystectomy is usually reserved for high-risk cases of non-muscle invasive bladder cancer that do not respond to other treatments. After cystectomy, the urine has to be diverted to an external bag or an internal pouch made from a piece of intestine.
Transurethral Resection of Bladder Tumor (TURBT)
Non Muscle Invasive Bladder cancer Treatment Options
Muscle Invasive Bladder Cancer Treatment
Surgery is the most common treatment for muscle invasive bladder cancer. The goal of surgery is to remove the tumor and any nearby lymph nodes that may be affected. There are two main types of surgery for MIBC: radical cystectomy and partial cystectomy.
- Radical cystectomy: involves removing the entire bladder and surrounding tissue. Prostate and seminal vesicles are also removed in men. In women uterus is also removed if associated closely with tumor, otherwise it can be preserved. lymph nodes in the pelvis are also removed on both sides.
- Urinary Diversion Procedures: After removing the bladder, the surgeon needs to create a new way for urine to leave the body. This is called urinary diversion. The most common types of urinary diversion are:
- Ileal conduit diversion: The surgeon uses a piece of small intestine (ileum) to make a tube that connects the ureters (the tubes that carry urine from the kidneys) to an opening (stoma) on the abdomen. The urine flows through this tube and out of the stoma into a bag that is attached to the skin. The bag needs to be emptied several times a day.
- Continent cutaneous diversion: This is also known as continent urinary diversion, because urine can be controlled and does not leak out of the body. The surgeon uses a piece of large intestine (colon) to make a pouch that stores urine inside the abdomen. The pouch is connected to a stoma on the abdomen by a valve that prevents urine from leaking out. The urine can be drained from the pouch by inserting a catheter (a thin tube) through the stoma several times a day.
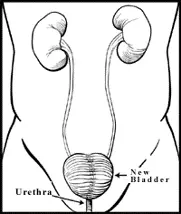
- Neobladder: This is also known as orthotopic neobladder, because it mimics the function of a normal bladder. The surgeon uses a piece of small intestine to make a new bladder that is attached to the urethra (the tube that carries urine out of the body). Urine passed out from body through urethra as in normal passage. The new bladder can store urine and be emptied by contracting the abdominal muscles or using a catheter.
The type of urinary diversion that is best for each person depends on many factors, such as their overall health, preferences, and care needs. The surgeon will discuss the advantages and disadvantages of each option with them before surgery.
- Partial Cystectomy: In small single tumor away from opening of ureter and bladder base, part of urinary bladder with adequate margin can be excised. Remaining bladder is repaired and lymph nodes in pelvis excised.
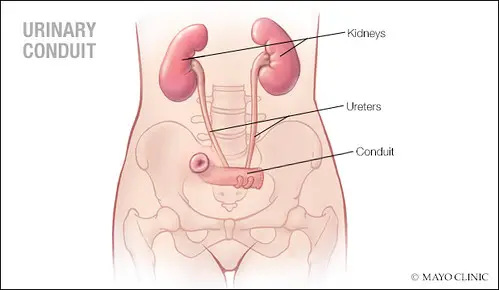
Ileal Conduit (Urostomy)
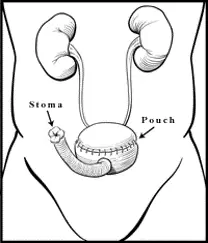
Continent Urinary Divesion
Neobladder
To Book Appointment for Cancer Surgery :
Integration of Multimodality Treatment
- Radiation therapy is a treatment that uses high-energy rays or particles to destroy cancer cells or stop them from growing. Radiation therapy may also be given as an alternative to surgery for patients who are not eligible or willing to undergo surgery.
Chemotherapy is a treatment that uses drugs to kill cancer cells or stop them from growing. Chemotherapy may be given before surgery (neoadjuvant chemotherapy) to shrink the tumor and make it easier to remove, or after surgery (adjuvant chemotherapy) to lower the chance of recurrence. Chemotherapy may also be given in combination with radiation therapy (chemoradiation) to enhance its effectiveness.
Bladder Preservation Protocol: Maximal TURBT + Radiation Therapy + Chemotherapy for muscle invasive bladder cancer preserve native bladder while curing the cancer in suitable patients.
Immunotherapy is a treatment that uses the body’s own immune system to fight cancer cells. Immunotherapy may be used alone or in combination with other treatments for MIBC.
Targeted therapy is a treatment that uses drugs that target specific molecules or genes that are involved in the growth and spread of cancer cells. Targeted therapy may be used alone or in combination with other treatments of metastatic bladder cancer.
Self Care Guide for Ileostomy
- Right after the surgery, don’t do anything strenuous. Follow your doctor’s instructions on when you can resume normal activities.
- Always wash your hands before touching the stoma or areas around the stoma.
- Washing around the stoma with water is enough, but you can use mild unscented soap if you want. Rinse well and pat dry gently.
- Check for any allergic reactions.
- Choose a pouch that fits well around your stoma and does not leak or irritate your skin.
- Change your pouch whenever it feels uncomfortable or full. Usually, you will need to change it every 5 to 7 days.
- Empty your pouch when it is about one-third full or before going to bed. To empty it, open the bottom of the pouch over a toilet or container and drain the urine. Rinse the pouch with water if needed and close it securely.
- Dispose of used pouches in a plastic bag and throw them away in the trash. Do not flush them down the toilet.
- Check your stoma regularly for any signs of infection, bleeding, swelling, or changes in color or size. Contact your doctor if you notice any problems or have any questions.
- Drink plenty of fluids (at least 8 glasses of water per day) to keep yourself hydrated and prevent urinary tract infections.
- Eat a balanced diet that includes enough fiber to prevent constipation.
Self Care Guide for Neobladder
You will need to learn how to empty your neobladder regularly and completely. Unlike your natural bladder, your neobladder does not have nerves that tell you when it is full or when you need to urinate. You will need to rely on a schedule and a watch to remind you when to go to the bathroom.
You will also need to use abdominal muscles and change positions to help squeeze out all the urine from your neobladder. Your doctor and nurse will teach you how to do this while you are in the hospital.
You may need to self-catheterize if you have trouble emptying your neobladder completely. This means inserting a catheter into your urethra and draining any leftover urine from your neobladder. This can prevent urinary retention, which can cause infection, kidney damage, or leakage of urine. Your doctor and nurse will teach you how to do this safely and hygienically.
You will need to avoid strenuous activities or lifting heavy objects for 4 to 6 weeks after your surgery. You can gradually resume your normal activities as you heal and feel better.
Got some questions
Urinary bladder, kidney/ renal pelvis and ureter cancers are grouped together because biology of all these is same in most of times which is urothelial carcinoma in 90% of cases. Contact Cancer Surgery clinic Arogyam Care at Gurugram, Delhi NCR or book online appointment for colon and rectal cancer treatment in Gurgaon.
- If all relavant examination and investigations has been done than plan of treatment is finalized with colon cancer surgeon
- After deciding surgical procedure cost estimate can be taken from billing department or hospital. Clinic or hospital department coordinator will assist in case any help required. +918750587489,
- Routine screening is not advised. Workers at high-risk industrial area should be advised routine health checkup including urine routine examination with cytology and cystoscopy if needed.
- You can consult us through our online consultation link. https://api.whatsapp.com/send/?phone=918750587489&text=I+am+Looking+for+an+appointment+with+Dr.+Kaushal+Yadav.+Please+Help&type=phone_number&app_absent=0
Non muscle invasive / superficial bladder can have good survival but has high recurrence rate so regular cystoscopy followup is advised. Muscle invasive bladder cancer treated with radical cystectomy can also reoccur as per stage of the disease.