Rectal Cancer
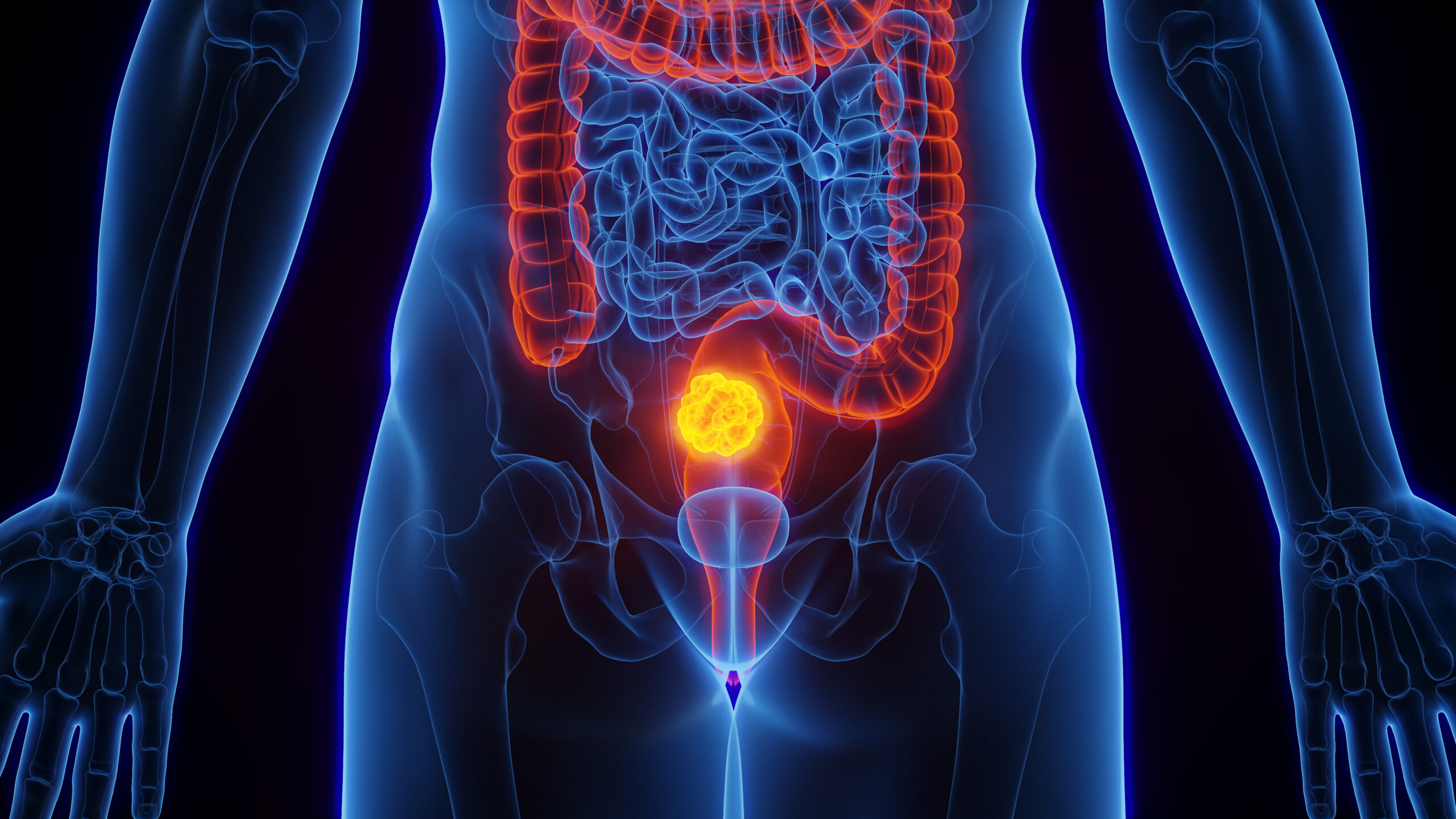
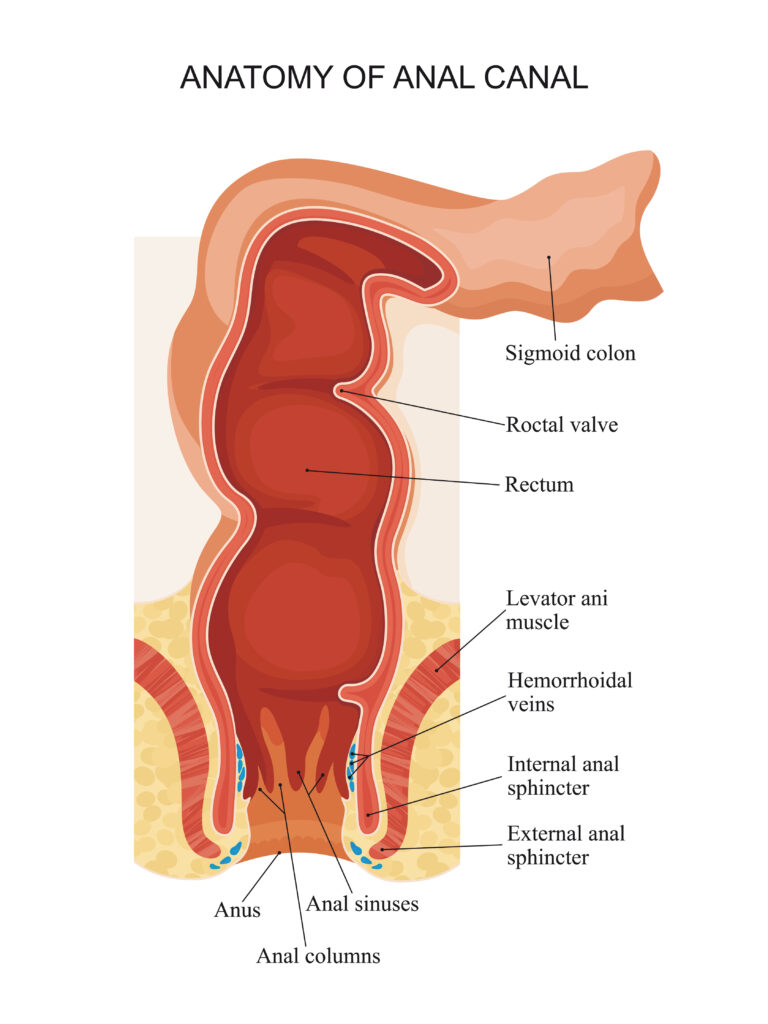
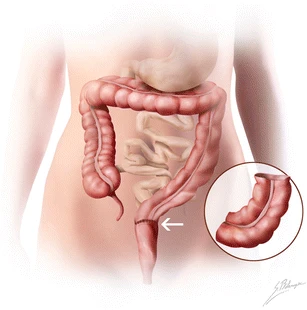
Rectal cancer is a type of cancer that starts in the lower part of the large intestine, called the rectum. Rectum is last part of large intestine. It holds stools before excreting them from body through anus. It has an important role in normal defecatory function of body. Colon continues in last part of large intestine called rectum, most of which is deep in pelvis. Food nutrients get absorbed in small intestine and residue reaches in colon where water is absorbed. The stool formed is hold in rectum untill passed out through anus. Understanding of anal sphincter is very important in management of rectum cancer and how to avoid colostomy or permanent stoma.
Colortectal cancers together are the 3rd most common cancer and 2nd most common cause of cancer related mortality globally. In India it is 6th most common cancer group and 7th most common cause of cancer related mortality.
Types
- Adenocarcinoma: The vast majority of colon cancers are adenocarcinomas. This type of cancer develops from cells that line the inside of the colon and rectum.
- Other types: these includes neuroendocrine tumors, which develop from hormone-producing cells, and gastrointestinal stromal tumors (GISTs), which develop from connective tissue cells in the GI tract.
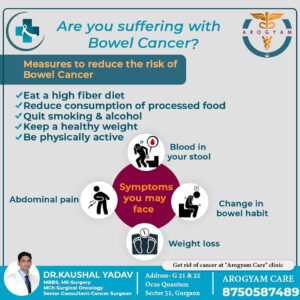
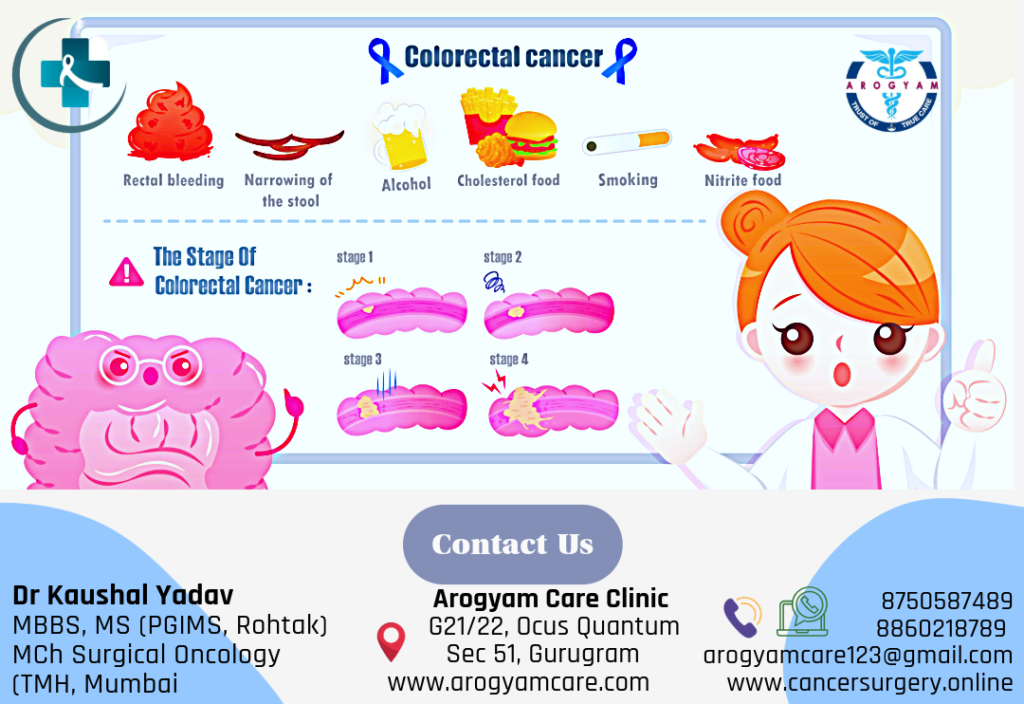
Risk Factors/ Causes of Rectum Cancer
- Age: the risk of rectum cancer increases with age. Most colon cancers are diagnosed in people over the age of 50.
- Personal or family history of colorectal cancer or polyps. Having had colon cancer or noncancerous growths called polyps in the past, or having a close relative with them, increases the risk of colorectal cancer.
- Diet: a diet high in fat and low in fiber can increase your risk of rectal cancer. Diets that include a lot of processed meat and red meat increase the risk of colon cancer. These dietary factors increase the risk of rectum cancer in 15-30% cases.
- Smoking: smokers are more likely to develop rectum cancer than non-smokers.
- Alcohol: heavy drinkers are at an increased risk for developing large intestine cancer.
- Obesity: people who are obese have an increased risk of developing rectum cancer.
- Being physically inactive/ sedentary
- Abdominopelvic radiation exposure
- Genetic mutations. Some inherited conditions, such as familial adenomatous polyposis (FAP) and Lynch syndrome, can cause changes in the DNA of the cells in the colon that make them more likely to become cancerous.
*Diet rich in fruits, vegetables, and whole grains, fibers and that limits or avoids red and processed meats and sugary drinks probably lowers risk.
Screening for Colorectal Cancer:
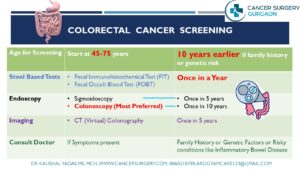 The American Cancer Society recommends that people with average risk should start regular screening at age 45. This can be done either with a stool based test to detect blood or by colonoscopy. People in good health should continue regular colorectal cancer screening up to 75 years. Between 76 – 85 years screening should be based on person’s preferences, overall health, and prior screening history. Beyond 85 years colorectal cancer screening usually not recommended.
The American Cancer Society recommends that people with average risk should start regular screening at age 45. This can be done either with a stool based test to detect blood or by colonoscopy. People in good health should continue regular colorectal cancer screening up to 75 years. Between 76 – 85 years screening should be based on person’s preferences, overall health, and prior screening history. Beyond 85 years colorectal cancer screening usually not recommended.
Usually recommended tests are:
- Stool Tests: Fecal Immunohistochemical Test (FIT) & Fecal Occult Blood test (FOBT) – Stool based test once a year can decrease colorectal cancer morality by 30%.
- Colonoscopy: Colonoscopy is an endoscopic examination to check inside of large intestine. Colonoscopy once in every 10 years decrease colorectal cancer related mortality by 50%.
- CT colonography (virtual colonoscopy) every 5 years in patients not opting colonoscopy as alternative method.
- Flexible sigmoidoscopy every 5 years.
For persons with high risk or family history of colon or rectum cancer screening and cancer checkup tests are recommended to start early and more frequently with advice from treating colorectal cancer surgeon for rectum cancer.
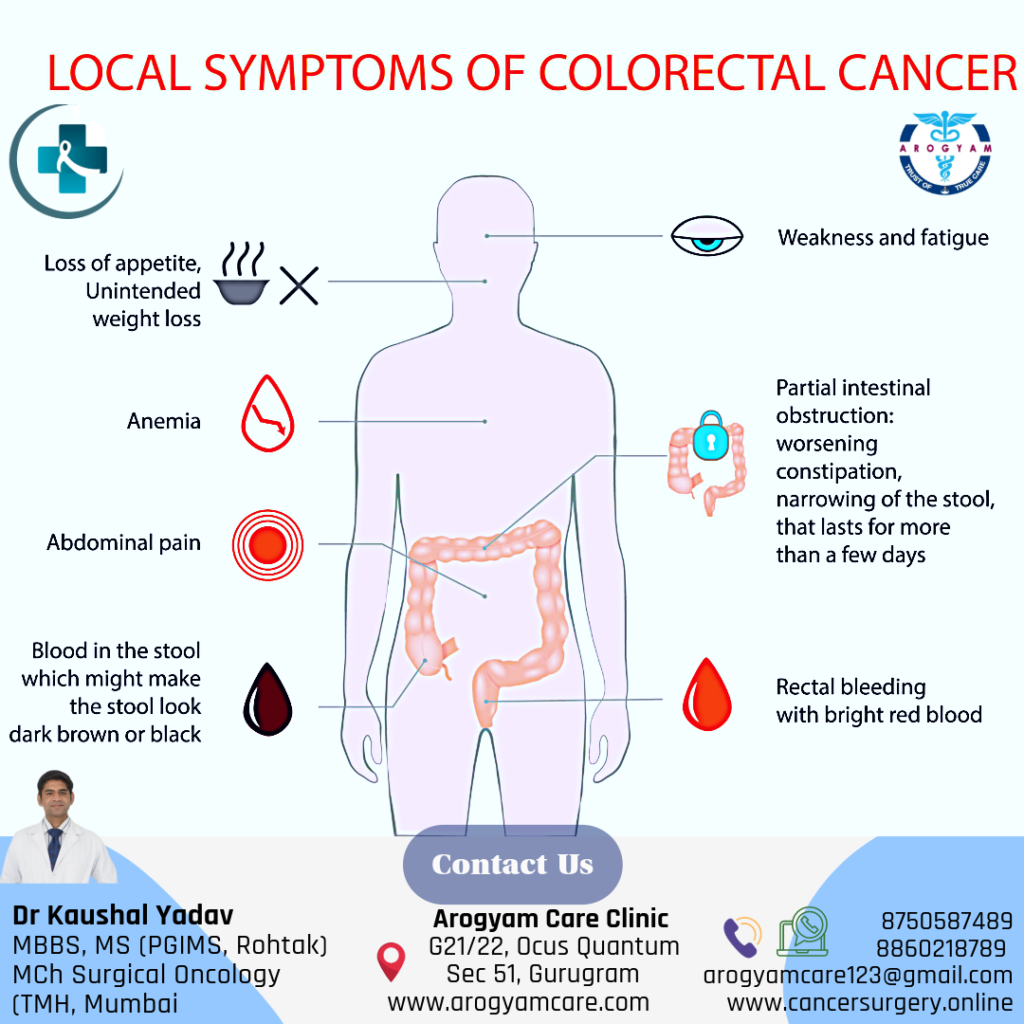
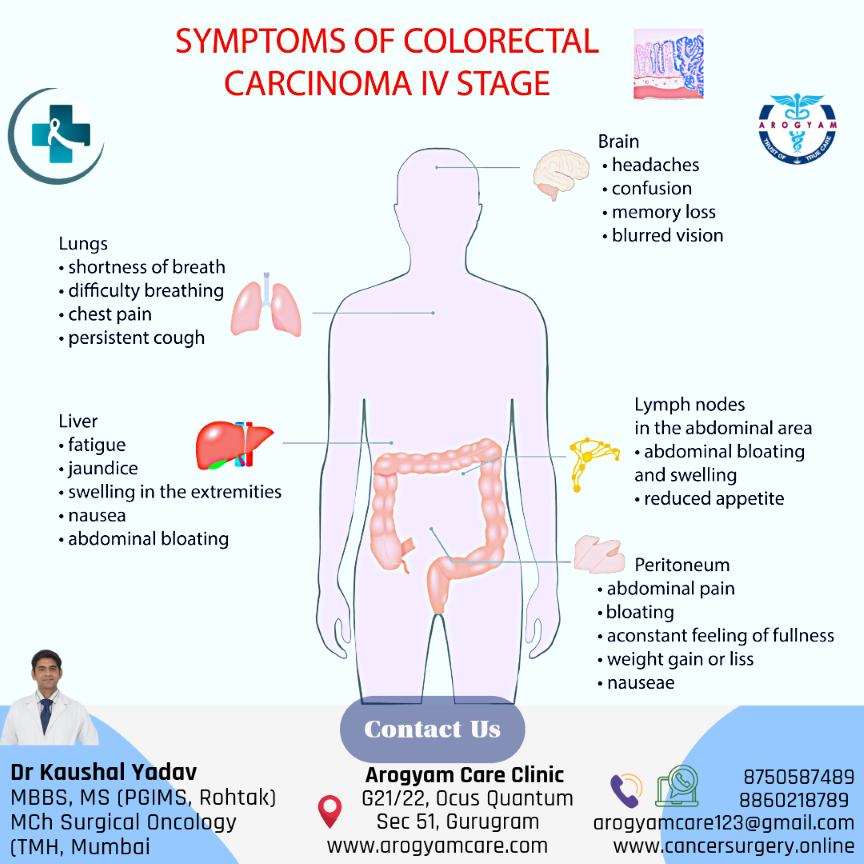
Alarming Signs and symptoms of Rectal Cancer
- Rectal Bleeding: The most common symptom of colorectal cancer is bleeding from the rectum or blood in the stool.
- A change in bowel habits, such as diarrhoea, constipation, or narrowing of the stool
- Pain in lower abdomen
- Weakness and fatigue
- Unexplained weight loss
- Urge of passing stools but not passing
- Urinary difficulty in case of bulky disease
Investigations
- Physical examination: The doctor will ask about your medical history and perform a physical exam. Physical examination is main assessment to determine distance between tumor and anal sphincter
- Colonoscopy: This uses a long, flexible tube with a camera and a light at the end (colonoscope) to examine the inside of your colon and rectum. The doctor can also take tissue samples (biopsies) or remove polyps (growths) during this test. The tissue samples are sent to a lab to be checked for cancer cells.
- Biopsy: a small piece of tissue removed from the tumor or polyp and examining it under a microscope. A biopsy confirms the diagnosis of rectal cancer.
 .
. - Blood tests: These measure the levels of tumor markers is carcinoembryonic antigen (CEA), which may be higher than normal in people with this disease.
- Imaging tests: PET CECT/ CT Scan/ MRI: Imaging tests show the size and location of the rectal tumor, as well as whether it has spread to nearby or distant organs. Contrast MRI Pelvis helps in identifying safety of stool controlling muscles (Sphincters). Based on tumor spread in relation with anal sphincters/ Levator ani muscle; it is decided whether patient can be treated with sphincter saving approach or not.
Treatment
Surgery is the most common treatment for rectal cancer. It involves removing the part of the rectum that contains the cancer, along with some surrounding normal tissue and lymph nodes. There are different types of surgery for rectal cancer, depending on the location and size of the tumor.
Sphincter Sparing Approaches: Sphincter-sparing approaches for rectal cancer refer to surgical techniques that aim to preserve the anal sphincter function while removing the cancerous tumor in the rectum. The goal is to avoid the need for a permanent colostomy, which is a surgical opening in the abdominal wall for the diversion of faeces. Complexities of sphincter-sparing procedures as cancer location goes more lower in rectum. Several sphincter-sparing surgical approaches are available for the treatment of rectal cancer, including:
- Transanal Endoscopic Microsurgery (TEM): TEM is a minimally invasive surgical technique performed through the anus using an endoscope and specialized instruments. It is suitable only for smallest possible cancer in the lower part of the rectum.
- Low Anterior Resection (LAR):The cancer bearing Segment of rectum with adequate margin of normal tissue around the cancer is removed, along with nearby lymph nodes and other tissues around the rectum. The colon is then reattached to the remaining rectum maintaining normal bowel function.
- Ultralow Anterior Resection (ULAR): remove the cancer in lower rectum while preserving the anal sphincter. The proximal colon is then reconnected to the anal canal, maintaining normal bowel function.
Short-term temporary stoma may be made in case of frail patients or difficult anastomosis. The end of the intestine is brought out through a hole in the skin of the abdomen. This gives the rectum time to heal before stool moves through it. Mostly stoma is reversed (the intestines reconnected) after adequate healing.
- Intersphicteric resection: In case of very low lying cancer where external anal sphincter (Levator ani muscle) is safe from disease and has adequate tone and normal margin can be taken distally. Proximal colon is anastomosed to anal canal. Temporary stoma is required and revered after healing of anastomosis
- Proctocolectomy with ileo-anal anastomosis: When there are multiple tumors/ polyps in colon and rectum complete colon and rectum is removed and small intestine is joined with anal canal.
It is essential to note that not all patients with rectal cancer are candidates for sphincter-sparing approaches. The treatment decision depends on various factors, including the stage and location of the tumor, the patient’s overall health, and the surgeon’s expertise. If you or someone you know is facing a diagnosis of rectal cancer, it is crucial to consult with a qualified surgical oncologist/ oncosurgeon to determine the most appropriate treatment plan.
Abdominoperineal Resection with Permanant Stoma: Cancer of lower part of the rectum or extending into anal canal, growing into the sphincter muscle (the muscle that keeps the anus closed and prevents stool leakage) or pelvic floor (called levator muscles). Also required in distal rectal cancer when sphincter muscle strength is poor.
Properly managed stoma gives better quality of life than uncontrolled and poorly managed anal passage.
Metastatectomy: if colon or rectal cancer has spread to limited organ like Liver or lung and complete excision of metastasis is possible.
Cytoreductive surgery + Hyperthermic Intraperitoneal chemotherapy(CRS+HIPEC): when there is peritoneal (inner covering of abdomen) only metastasis extensive surgery is done to completely remove the disease followed by intraperitoneal instillation of heated chemotherapy during surgery.
To Book Appointment for Cancer Surgery :
Integration of Multimodality Treatment
- Chemotherapy: is the use of drugs to kill cancer cells or stop them from growing. It can be given before or after surgery, or along with radiation therapy. Chemotherapy can help shrink the tumor before surgery, lower the risk of cancer coming back after surgery, or treat cancer that has spread to other parts of the body. The most common chemotherapy drugs used for rectal cancer are 5-fluorouracil (5-FU) and capecitabine (Xeloda). They are often given with a drug called leucovorin, which helps them work better.
- Radiation therapy is the use of high-energy rays or particles to destroy cancer cells or stop them from growing. It can be given before or after surgery, or along with chemotherapy. Radiation therapy can help shrink the tumor before surgery, lower the risk of cancer coming back after surgery.
- Targetted Therapy: have important role in advance/ metastatic disease. where medicine is given for specific receptors (targets) of cancer
- Immunotherapy: Acts with immune check points of cells and its role is emerging in colorectal cancer in specific patients.
STOMA: All you need to know about.
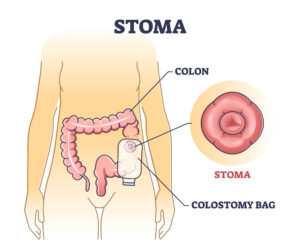 Stomas are surgically created openings in the abdominal wall that allow the diversion of faeces or urine when the normal route of elimination is not possible. The two main types of stomas related to the digestive system are colostomy and ileostomy, and they can be either permanent or temporary, depending on the underlying medical condition and the planned surgical approach.
Stomas are surgically created openings in the abdominal wall that allow the diversion of faeces or urine when the normal route of elimination is not possible. The two main types of stomas related to the digestive system are colostomy and ileostomy, and they can be either permanent or temporary, depending on the underlying medical condition and the planned surgical approach.Colostomy: A colostomy is a surgical procedure in which a portion of the colon (large intestine) is brought to the surface of the abdomen to create a stoma. The end of the colon is then connected to the stoma, allowing stool to pass directly from the colon out of the body through the stoma.
- End Colostomy: The stoma is created from the proximal end of the colon, and the distal part is either removed or sewn shut. Stool consistency depends on the location of the stoma, with end colostomies closer to the rectum producing more formed stool.
- Loop Colostomy: In this type, a loop of the colon is brought to the abdominal surface. A temporary opening is created in the loop to allow stool to pass
Ileostomy: An ileostomy involves bringing the end of the small intestine (ileum) to the abdominal surface to create a stoma. This allows the elimination of stool from the small intestine directly through the stoma.
Temporary and Permanent:
Permanent Stoma: is done when the lower part of the colon or the rectum is removed and anal sphincters are weak or removed.
Temporary stoma: is done when the lower part of the colon or the rectum needs time to heal after an injury, infection, inflammation, or surgery. A temporary stoma can be reversed by reconnecting the bowel ends.
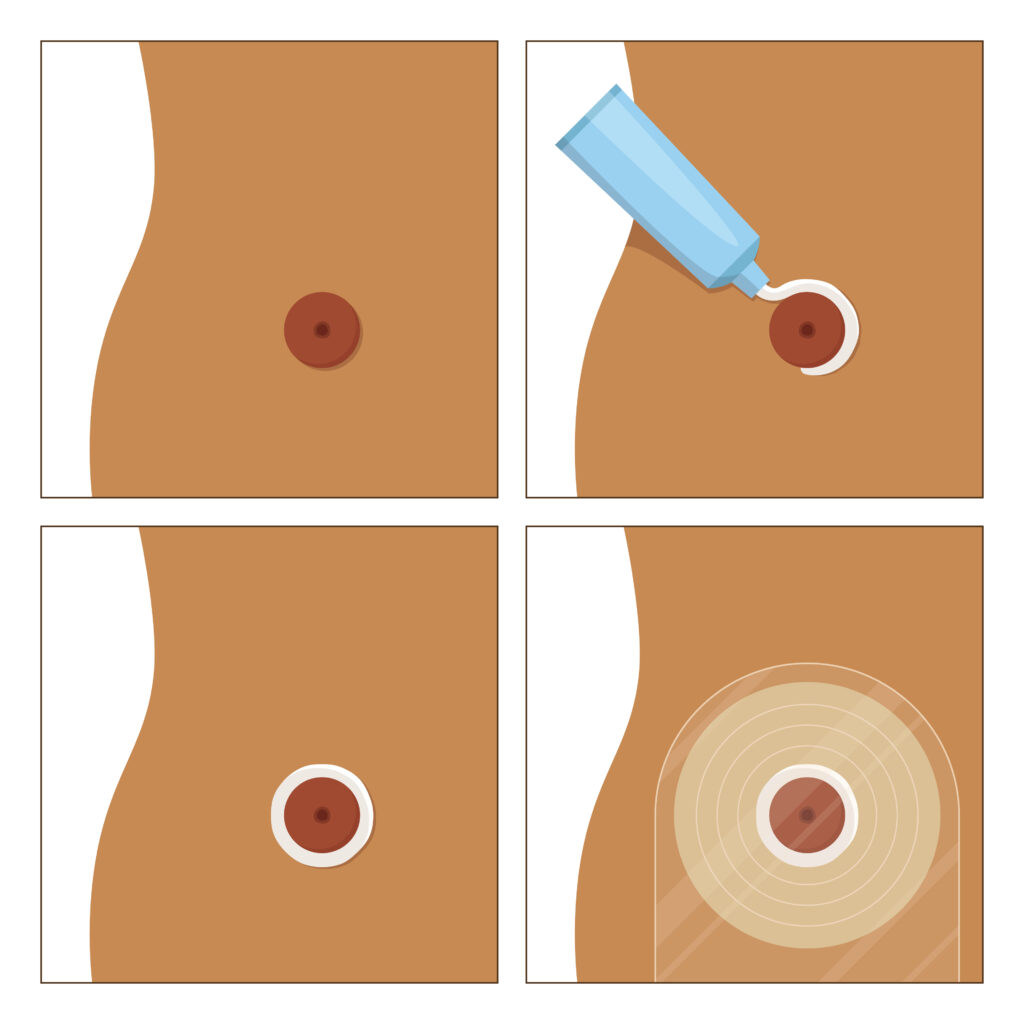
Care of Stoma: Your Guide of Self care
– Keep the stoma area clean and dry. Gently wash with warm water and a soft cloth during bathing. Avoid using soap, alcohol, or other harsh chemicals directly on the stoma.
– Observe the stoma regularly for any changes in size, color, or appearance. Report any unusual findings to your healthcare provider.
– Use a stoma powder or skin barrier wipe, if necessary, to protect the skin around the stoma from irritation.
- Ostomy Pouch Management:
– The stoma will continuously produce stool or mucus (in the case of colostomies), or liquid stool (in the case of ileostomies). These waste materials are collected in an ostomy pouch that adheres to the skin around the stoma.
– Empty the pouch when it is about one-third to one-half full to prevent it from becoming too heavy or causing leakage.
– Replace the pouching system regularly, following the instructions provided by the manufacturer or healthcare provider.
– Consider using specialized pouches for activities like swimming or other physical activities to ensure a secure fit.
- Diet and Hydration:
– Drink plenty of fluids and eat a balanced diet to keep your stools soft and regular. Regulate foods that can cause gas, odor, diarrhea, or constipation, such as beans, cabbage, broccoli, spicy foods, dairy products, nuts, seeds, popcorn, etc.
– Chew your food well and avoid swallowing air when you eat or drink. This will help prevent gas and bloating.
– Be active and exercise regularly to improve your blood circulation and digestion. You can do most activities with a stoma as long as you are careful and comfortable.
In conclusion, having a stoma can change your life in many ways, but it does not have to stop you from living well. By learning about the different types of stomas and how to take care for them, you can manage your condition and enjoy your daily activities. Remember that you are more than your stoma and that you can still do the things you love with some adjustments and precautions. If you have any questions or concerns about your stoma, do not hesitate to contact your doctor or nurse for guidance and advice.
How to Change Stoma Bag
Kiegel Exercises: Pelvic Floor Exercises
Related Video
Got some questions
- If all relavant examination and investigations has been done than plan of treatment is finalized with colon cancer surgeon
- After deciding surgical procedure cost estimate can be taken from billing department or hospital. Clinic or hospital department coordinator will assist in case any help required. +918750587489,
- you can visit nearby hospital for colonoscopy screening as advised in our screening section or you can read various society guidelines like American cancer society, USPTF.
- You can consult us through our online consultation link. https://api.whatsapp.com/send/?phone=918750587489&text=I+am+Looking+for+an+appointment+with+Dr.+Kaushal+Yadav.+Please+Help&type=phone_number&app_absent=0
Even in lowest of rectum cancer it is possible to preserve normal function. Requirement is that external sphincter (levator ani muscle) plane is safe and sphincters have good strength. Lowest margin during surgery is confirmed as negative for cancer cells on frozen section.
Lower the rectum cancer, more are chances of stoma (Colostomy/ ileostomy). In most cases stoma is temporary and usually closed after healing. In cases when sphincter is involved by disease, poor strength of muscles or disease is very bulky and negative margins not achievable than, permanent stoma is made after removing all pelvic disease.