Cervix Cancer
Cervix is lower part of uterus, and it connects uterus with vagina. Cervix or cervical cancer arises in the cell linings of cervix.
- Third most common and second most cancer common among female cancers in India.
- Account for 18.3% cases of female cancers and 9.4% of all cancer cases in India.
- Second most common cause of cancer related deaths in India
- World over trend of cervical cancer is decreasing due to proper adoption of hygienic practices and regular screening.
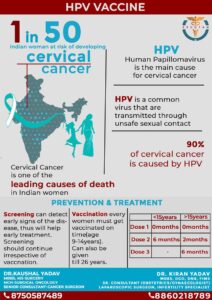
- New case detected of cervix cancer in India- 123 907 every year. 1 in 50 women is at risk of developing cervix cancer.
- 21% of all cases and 23% of all deaths related to cervix cancer occur in India. Study Link
Types of cervical cancer
- Squamous Cell Carcinoma: most common type 70-90%. Human papillomavirus (HPV) infection is a significant risk factor for the development of squamous cell carcinoma of cervix.
- Adenocarcinoma: This type accounts for approximately 10-20% of cervical cancers. It originates in the glandular cells of the cervix that produce mucus. Adenocarcinoma has been associated with certain subtypes of HPV and is often more difficult to detect and diagnose in its early stages compared to squamous cell carcinoma.
- Adenosquamous Carcinoma: This is a combination of adenocarcinoma and squamous cell carcinoma.
- Neuroendocrine Carcinoma (Small Cell Carcinoma): rare and aggressive type.
- Clear Cell Carcinoma
Risk Factors for developing cervical cancer
It isn’t clear what causes cervical cancer, but it’s certain that HPV plays a role. HPV is very common, and most people with the virus never develop cancer. This means other factors — such as your environment or your lifestyle choices — also determine whether an individual will develop cervical cancer.
- Many sexual partners, early sexual activity or high risk partner.
- Multiple pregnancies
- Other sexually transmitted infections, chlamydia
- Low immunity like in AIDS, immunosuppressive drugs
- Smoking
- Unhygienic menstrual practices
*HPV vaccination, safe sexual practices, pap smear screening and improving menstrual hygeine are important factors leading to decrese in cervix cancer cases
Screening for Cervix/ Cervical Cancer:
Screening helps in early detection and treatment. Screening helped a lot a decreasing the incidence and mortality rate of cervical cancer. It is most effective way to reduce the burden of this disease, and everyone should be educated regarding potential benefits.
The U.S. Preventive Services Task Force (USPSTF) recommends cervical cancer screening:
- 21-29 years, every 3 years with cervical cytology alone.
- 30 -65 years, every 3 years with cervical cytology alone, every 5 years with high-risk human papillomavirus (hrHPV) testing alone, or every 5 years with hrHPV testing in combination with cytology (cotesting).
Vaccination for cervix cancer
Vaccines are available against most commonly linked HPV types. It should be noted that these vaccines only prevent infection and doesn’t treat infection. To be most effective they should be given before onset of sexual activities. HPV vaccination is recommended for children between 9-12 years. Young teens and adults can be vaccinated up to 26 years, beyond which it is usually not recommended.
No vaccine provides complete protection against all HPV types. Regular cervical cancer screening should be continued as recommended despite vaccination.
Read more about HPV vaccination
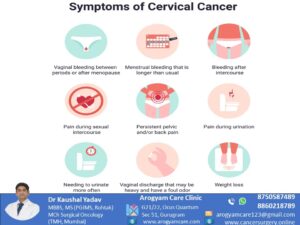
Alarmimg Signs and symptoms of Cervix Cancer
Oncologists treating cervical cancer advice regarding following sympltoms:
Investigations for diagnosis of cervix cancer
Colposcopy. Read More here
Biopsy
Ultrasound
MRI Pelvis- provide better extent of disease in surrounding soft tissues
CT scan/ PET CT- helps to assess extent of nearby and distant disease.
Cystoscopy/ colonoscopy/ examination under anesthesia – can be planned as per requirement for proper disease staging.
Stages of cervical cancer
Stage Ia: Microscopic disease in cervix
Stage III: Spread till pelvic wall, involve ureter or lymph nodes
Stage Ib : Grossly visible early disease in cervix only
Stage IVa: Involve rectum/ bladder
Stage IIa: Upper vagina involved
Stage IVb: Spread to distant organs
Stage IIb: Disease spread in nearby parametrium tissue
cervical cancer stages by Cancer Research UK href=”https://creativecommons.org/licenses/by-sa/4.0/” target=”_blank” rel=”noopener noreferrer”>CC BY-SA 4.0
Treatment of cervical cancer
Surgery for cervix cancer – is preferred curative option for early stage cervical cancer upto stage IIa.
- Radical Hysterectomy with Lymph node excision: Open approach is gold standard; minimal invasive approach can be considered for very small lesions. In radical hysterectomy tissue around uterus and cervix is also removed. This tissue is called as parametrium and ureters (tubes which carries urine from kidney to urinary bladder) passes through it. Parametrial tissue is removed, and ureters are saved, and nerve supply of bladder is also tried to be saved. This is a complex surgery and should be performed by cancer surgeon because an inadequately performed surgery will require further treatment. Radical hysterectomy is the
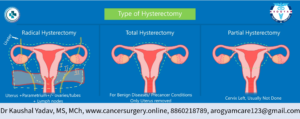 only treatment required in early stages. Surgical oncologist can perform this radical hysterectomy with good survival rates and early recovery.
only treatment required in early stages. Surgical oncologist can perform this radical hysterectomy with good survival rates and early recovery. - Fertility Sparing Surgery- Radical Trachelectomy – may be considered in selected early cases desiring future childbearing. Remove only cervix and preserve upper part of uterus which is sutured to vagina
- Pelvic Exenteration: is usually done in certain advance locoregional disease after chemoradiation failure. Extent of surgery is decided as tumor extent.
- Surgery for precancerous lesions include cone excison/ simple hysterectomy
Pelvic Exentration Surgery for recurrent cases of carcinoma cervix or carcinoma rectum
Complete Pelvic Exentration Surgery
Posterior Exentration, Bladder saved
Anterior Exentration, Rectum saved
by Cancer Research UK is licensed under <a href=”https://creativecommons.org/licenses/by-sa/4.0/” target=”_blank” rel=”noopener noreferrer”>CC BY-SA 4.0</a>
To Book Appointment for Cervix Cancer Surgery :
Integration of Multimodality (Chemotehrapy, Radiotherapy) Treatment for cervical cancer
- Radiation Therapy – Preferably give along with chemotherapy as definitive chemoradiatherapy for large tumors and advance stage IIb onwards.
- Chemotherapy – usually given along with radiation therapy or in metastatic disease as palliative.
Related Video
Got some questions
With regular screening it is possible to detect cervix cancer in early stages. Sexually active females between 21-65 years should do conventional pap smear every 3 years or Pap smear with HPV DNA every 5 years.
- When detected early, it is possible to do Radical Hysterectomy surgery, which has a very good cure rate.
- In advance case Radiation therapy is also helpful in curing the disease
- Only those cases which present in last or metastatic disease cannot be cured completely.
- So if timely treatment taken cervix cancer is curable
Conventional pap smear costs around 300-500 INR per 3 year, Pap with HPV DNA costs around 3000-5000 INR per 5 years. Even more cost affordable test of visual inspection under acetic acid is available. So with a small cost of screening lacs of treatment cost can be saved.
Ideal age for HPV vaccination is 9-14 years. 15-26 years is another suitable group. After 26 years very less advantage.
Minimal Invasive approaches of surgery like laparoscopy and robotic surgery are at present found to be inferior to open radical hysterectomy. So; till good level of evidence becomes available, it is advisable to perform this surgery by open approach.