Ovarian Cancer : hidden enemy on rise.
Every year, nearly 48,000 Indian women receive an ovarian cancer diagnosis—about one in every 15,000. That fraction may seem small, but in a nation of hundreds of millions, each case represents a life story, a family in turmoil, and dreams put on hold. Understanding the full picture is the first step toward action.
The Hidden Scale of a Silent Threat
Ovarian cancer ranks as the third most common malignancy among Indian women.
- Annual new cases: ~48,000
- Ratio: 1 in 15,000 women
In densely populated cities, that “tiny” fraction becomes painfully visible. Every dot on the map represents a daughter, a sister, or a friend whose future hangs in the balance.
A Younger Demographic at Risk
In India, ovarian cancer strikes at a younger age than in Western countries.
- Median age at diagnosis: 41–54 years
- Many cases occur in women under 50
Careers, families, and new life chapters can be disrupted just as they’re taking off. Raising awareness among women in their 30s and 40s is critical for early action.
What Drives Ovarian Cancer? Four Key Causes
- Genetics and Family History
About 20% of ovarian cancers stem from inherited mutations. The BRCA genes are the most notorious:
|
Mutation |
Lifetime Ovarian Cancer Risk |
|
BRCA1 |
40–60% |
|
BRCA2 |
10–30% |
If breast or ovarian cancer runs in your family, discuss genetic testing in India. Early insight can guide surveillance, preventive surgery, or targeted lifestyle changes.
- Hormones and Reproductive Choices
Modern trends in childbirth and menopause shift hormone exposure:
- Delayed first childbirth and fewer pregnancies reduce natural protection
- Early periods or late menopause increase lifetime estrogen exposure
- Hormone replacement therapy (HRT) adds to the risk
Yet certain choices cut risk:
- Oral contraceptives for ≥5 years lower risk by 30–50%
- Breastfeeding offers additional hormone regulation
- Incessant Ovulation
Every ovulation cycle causes tiny damage to ovarian cells. With over 400 cycles in a lifetime, that cumulative “wear and tear” raises cancer risk—like water slowly carving stone.
- Endometriosis
Women with endometriosis have up to a 4× higher risk of ovarian cancer. This condition is more than painful cramps; it’s a signal to maintain vigilant health monitoring and regular screenings.
Rising Trend in Urban India
Ovarian cancer cases in urban centers have been climbing by 1–2% each year. Changing lifestyles, stress, and environmental pollutants may all play a role. Every percentage point represents more lives affected, underscoring the need for evolving awareness and screening efforts.
Lifestyle Factors You Control
While you can’t change your DNA, you hold the reins on daily habits that influence risk:
- Overweight women face a 20–30% higher risk
- Diets high in fat and frequent egg consumption can drive insulin resistance and chronic inflammation
- Smoking is a confirmed risk factor; alcohol’s role is under study
- Chronic pelvic infections or PCOS add to inflammation
- Dairy is a double-edged sword:
- Low-fat milk, calcium, and vitamin D may lower risk
- High-estrogen dairy products (including hormone-boosted paneer) could raise risk
Modifiable lifestyle choices:
- Embrace a high-fiber, plant-rich diet
- Choose lean proteins and low-estrogen dairy
- Avoid smoking and drink alcohol sparingly
- Keep a healthy weight through balanced meals and regular exercise
Every healthy habit compounds into powerful protection.
Early Detection: Your Best Defense
Known as the “silent killer,” ovarian cancer often presents with subtle symptoms. But if caught early, the five-year survival rate jumps above 90%. Key steps:
- Listen to your body: persistent bloating, pelvic discomfort, or urinary changes for more than a few weeks deserve attention.
- Share concerns with your doctor: no symptom is too small to discuss.
- Consider targeted screening: for those with genetic risks, transvaginal ultrasounds and CA-125 blood tests can offer an early warning.
Timing is everything. Detect early, fight stronger, and rewrite your story.
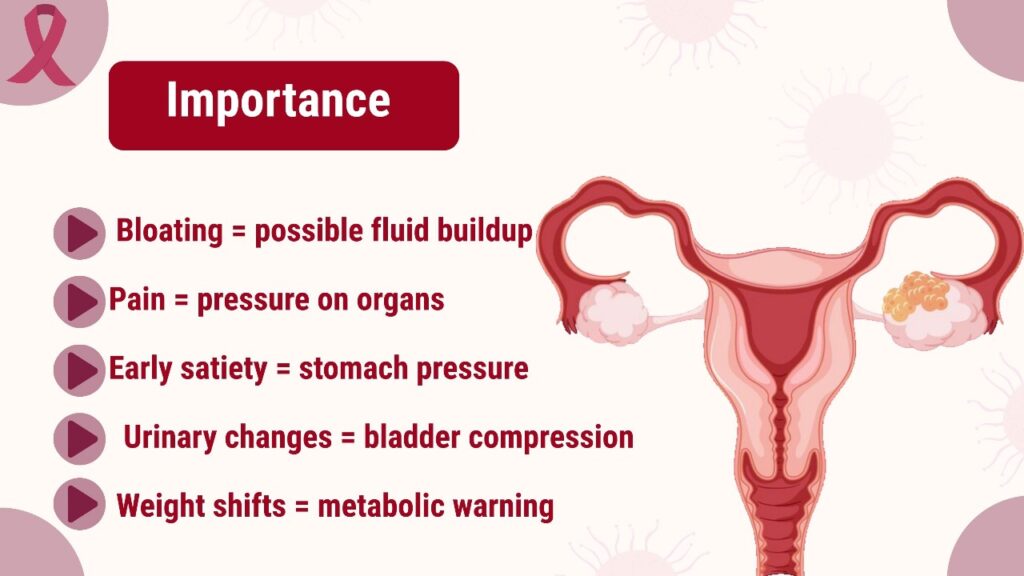
Spot the Early Warning Signs
Below are symptoms that should never be ignored, along with why they matter and when to take action:
- Persistent abdominal bloating
• Why it matters: Unresolved bloating for more than two weeks can signal fluid buildup (ascites) or an enlarging ovarian mass.
• When to act: Track its duration and if your waistline inches up without diet changes—schedule a check-up. - Pelvic or lower back pain
• Why it matters: A tumor pressing on pelvic nerves or organs often causes dull aches or sharp pains.
• When to act: If over-the-counter painkillers only mask discomfort and it becomes part of your daily routine, consult a doctor. - Feeling full quickly (early satiety)
• Why it matters: Pressure on the stomach from an ovarian growth can make small meals overly satisfying.
• When to act: Note if normal portions leave you uncomfortably full repeatedly—keep a food diary and discuss it during your next visit. - Frequent or urgent urination
• Why it matters: An ovarian tumor can press against the bladder, cutting its capacity and triggering constant trips.
• When to act: If you’re rushing to the restroom multiple times daily—despite usual fluid intake—investigate further with your physician. - Unexplained weight changes
• Why it matters: Sudden weight gain may come from fluid retention; rapid weight loss can result from metabolic shifts as your body battles disease.
• When to act: Weigh yourself weekly—any unexplained shift beyond 2–3% of your body weight over a month warrants medical advice.
Recommended Screening Guidelines (American Cancer Society)
-
ovarian cancer screening: American cancer society (ACS) advise on ovarian cancer screening · CA-125 · transvaginal ultrasound · high-risk ovarian cancer
While early detection is key, the American Cancer Society does not recommend routine ovarian cancer screening for women at average risk. Here’s what ACS advises:
- No routine CA-125 blood tests or transvaginal ultrasounds for asymptomatic, average-risk women
• Why: These tests have a high rate of false positives, leading to unnecessary invasive procedures and anxiety. - Pelvic exam is not a reliable screening tool for ovarian cancer
• Women should continue regular gynecologic check-ups but understand that a normal pelvic exam does not rule out early disease. - Women at high genetic risk (BRCA1/2 mutations or a strong family history) should seek genetic counseling
• Genetic counselors can recommend personalized surveillance, which may include CA-125 and transvaginal ultrasound starting at age 30–35 or 5–10 years earlier than the youngest affected relative.
• Risk-reducing surgery (bilateral salpingo-oophorectomy) may be discussed as the most effective prevention strategy for mutation carriers.
Symptom awareness remains your best screening tool
• Because formal screening isn’t effective for average-risk women, knowing and acting on persistent warning signs—bloating, pelvic pain, early fullness, urinary changes—offers the most practical early detection approach.Armed with this guidance, high-risk women can partner with their Oncologist/ Doctor/ Gynecologist on tailored surveillance, while all women stay alert to early warning signs. Remember: in the absence of a reliable population-wide screening test, knowledge and vigilance are your strongest defenses.
- No routine CA-125 blood tests or transvaginal ultrasounds for asymptomatic, average-risk women
Related Video
To Know more about cancer prevention
Discover more from CancerSurgery
Subscribe to get the latest posts sent to your email.