Pancreatic cancer is relatively uncommon, at no 24th in incidence; but >90% mortality rate in India. It means most of patients diagnosed with pancreas cancer will die from it. There is only one hope and that is to identify and operate it at earliest possible stage. Surgery is the only treatment modality which has shown good survival rates in pancreas cancer. Pancreas can is mostly undetectable initially, rapidly growing aggressive tumour with high recurrence rates. There are no initial symptoms because it is located deep inside abdomen and there is no routine screening test for pancreas cancer. Normal routine health checkup is not sufficient to detect pancreas cancer early. So it can be called as “Silent and Deadly Cancer”.
Pain Abdomen

Jaundice
Loss of weight

New Onset Diabetes

weakness and loss of energy

Itching with Jaundice
Understanding Pancreatic Cancer: Causes, Symptoms, and Treatment
Pancreatic cancer is a type of cancer that begins in the tissues of the pancreas, an organ located behind the lower part of the stomach. The pancreas plays a crucial role in digestion and regulating blood sugar levels by producing enzymes and hormones, such as insulin. Pancreatic cancer is often referred to as a “silent disease” because it typically presents with few symptoms until it is in advanced stages, making early detection challenging. Understanding the causes, recognizing the symptoms, and exploring the treatment options is essential for managing this aggressive cancer.
Causes of Pancreatic Cancer
The exact cause of pancreatic cancer is not always clear, but several risk factors are associated with an increased likelihood of developing the disease:
Genetic Mutations: Changes in the DNA of pancreatic cells can lead to uncontrolled growth and cancer. Some people inherit gene mutations that increase their risk of pancreatic cancer, such as mutations in the BRCA2 gene.
Family History: Having a family history of pancreatic cancer or other cancers, such as breast or ovarian cancer, can increase the risk.
Chronic Pancreatitis: Long-term inflammation of the pancreas, often due to heavy alcohol use or genetic disorders, is associated with an increased risk.
Diabetes: There is a link between type 2 diabetes and pancreatic cancer, although the exact nature of this relationship is still under study.
Smoking: Cigarette smoking is a major risk factor for pancreatic cancer, with smokers being twice as likely to develop the disease compared to non-smokers.
Obesity: Excess body weight, particularly abdominal fat, has been linked to a higher risk of pancreatic cancer.
Age: The risk of pancreatic cancer increases with age, with most cases occurring in people over 65.
Diet: A diet high in red and processed meats and low in fruits and vegetables may increase the risk of pancreatic cancer.
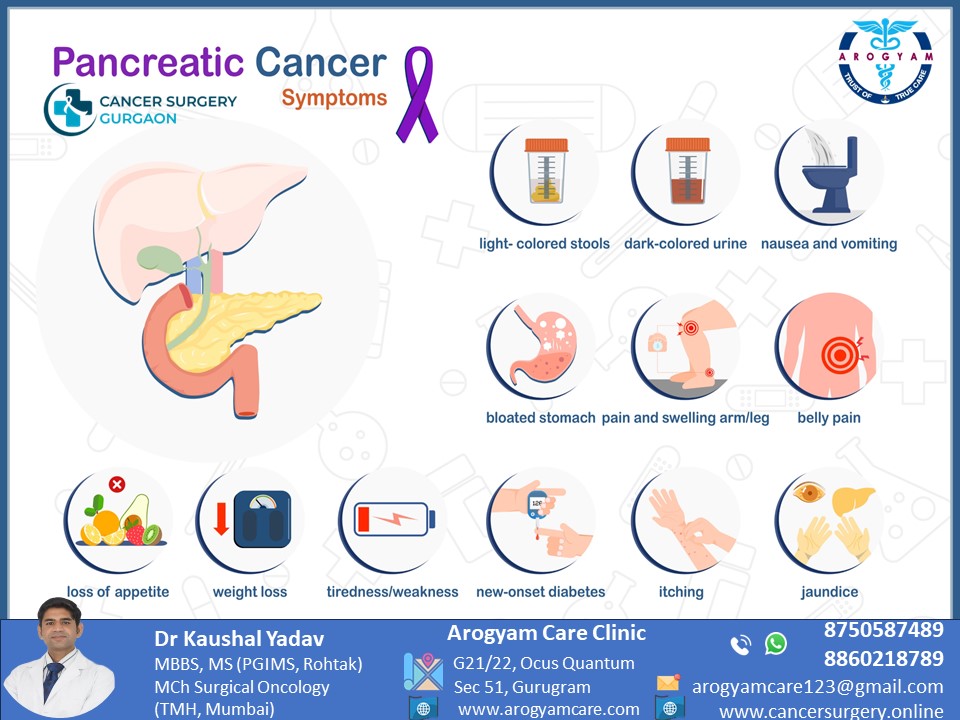
Symptoms of Pancreatic Cancer
Pancreatic cancer symptoms often do not appear until the cancer is advanced, making early detection difficult. Common symptoms include:
Jaundice: Yellowing of the skin and eyes, along with dark urine and pale stools, is often one of the first signs of pancreatic cancer. This occurs because the tumor can block the bile duct.
Abdominal or Back Pain: Pain in the upper abdomen or back may occur as the cancer grows and presses on surrounding organs or nerves.
Unexplained Weight Loss: Sudden and unintentional weight loss can be an early sign of pancreatic cancer, often due to loss of appetite or the body’s inability to absorb nutrients.
Loss of Appetite: Many people with pancreatic cancer experience a lack of appetite or a feeling of fullness after eating small amounts.
Nausea and Vomiting: As the tumor grows, it can block the stomach or intestines, leading to nausea and vomiting.
New-Onset Diabetes: In some cases, pancreatic cancer can cause diabetes, as the cancer affects the pancreas’s ability to produce insulin.
Fatigue: Persistent and unexplained fatigue is common in people with pancreatic cancer.
Diagnosis of Pancreatic Cancer
Diagnosing pancreatic cancer often involves several tests to confirm the presence of cancer and determine its stage:
Imaging Tests:
- CT Scan: Provides detailed images of the pancreas and surrounding organs to identify tumors.
- MRI: Offers high-resolution images to help detect pancreatic cancer.
- Endoscopic Ultrasound (EUS): Combines endoscopy and ultrasound to obtain detailed images of the pancreas and guide biopsies.
- Positron Emission Tomography (PET) Scan: Used to detect cancer spread beyond the pancreas.
Biopsy: A sample of pancreatic tissue is taken and examined under a microscope to confirm the presence of cancer cells.
Blood Tests: Blood tests may include measuring levels of tumor markers, such as CA 19-9, which can be elevated in people with pancreatic cancer.
ERCP (Endoscopic Retrograde Cholangiopancreatography): This procedure uses a dye to highlight the bile ducts on X-ray images, helping to identify blockages caused by tumors.
Staging of Pancreatic Cancer
Staging describes the extent of cancer spread and is crucial for determining treatment options:
- Stage 0: Cancer is confined to the top layers of pancreatic duct cells and has not spread. Known as carcinoma in situ.
- Stage I: Cancer is limited to the pancreas and is small (less than 2 cm for stage IA and between 2-4 cm for stage IB).
- Stage II: Cancer may be larger or have spread to nearby tissues and lymph nodes but has not spread to distant sites.
- Stage III: Cancer has spread to major blood vessels near the pancreas and may have spread to lymph nodes.
- Stage IV: Cancer has spread to distant organs, such as the liver or lungs.
Treatment Options for Pancreatic Cancer
Treatment for pancreatic cancer depends on the stage, location of the tumor, and the patient’s overall health. Common treatment options include:
Surgery: Surgery aims to remove the tumor and is most effective for early-stage pancreatic cancer.
- Whipple Procedure (Pancreaticoduodenectomy): The most common surgery for pancreatic cancer, it involves removing the head of the pancreas, part of the small intestine, gallbladder, and a portion of the bile duct.
- Distal Pancreatectomy: Removes the body and tail of the pancreas and sometimes the spleen.
- Total Pancreatectomy: Removes the entire pancreas, along with parts of the stomach, small intestine, and other nearby organs.
Radiation Therapy: Uses high-energy rays to kill cancer cells and shrink tumors. It can be used before surgery to reduce tumor size or after surgery to target remaining cancer cells.
Chemotherapy: Involves using drugs to kill cancer cells. It can be used alone or in combination with other treatments to control cancer growth, shrink tumors before surgery, or kill remaining cancer cells after surgery.
Targeted Therapy: Uses drugs that specifically target abnormalities in cancer cells. For example, Erlotinib is a targeted therapy used to treat pancreatic cancer with specific genetic mutations.
Immunotherapy: Helps the immune system recognize and attack cancer cells. Some forms of pancreatic cancer with specific genetic markers may respond to immunotherapy.
Palliative Care: Focuses on relieving symptoms and improving the quality of life for patients with advanced pancreatic cancer. It includes pain management, nutritional support, and psychological counseling.
Living with Pancreatic Cancer
Living with pancreatic cancer can be challenging, but support is available to help manage the disease and maintain quality of life:
- Nutrition: Eating a balanced diet and managing symptoms like nausea and loss of appetite are crucial for maintaining strength during treatment.
- Pain Management: Effective pain control is essential for improving comfort and quality of life.
- Emotional Support: Counseling, support groups, and mental health services can provide emotional support and help patients and families cope with the impact of cancer.
- Follow-Up Care: Regular follow-up appointments are essential to monitor for cancer recurrence and manage any long-term effects of treatment.
Prevention of Pancreatic Cancer
While not all cases of pancreatic cancer can be prevented, certain lifestyle changes can help reduce the risk:
- Quit Smoking: Smoking is a significant risk factor for pancreatic cancer. Quitting smoking reduces the risk.
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight through diet and exercise can reduce the risk of pancreatic cancer.
- Healthy Diet: A diet rich in fruits, vegetables, and whole grains, with limited red and processed meats, may lower the risk.
- Limit Alcohol Consumption: Heavy alcohol use can increase the risk of chronic pancreatitis, a risk factor for pancreatic cancer.
- Regular Medical Check-ups: For individuals with a family history of pancreatic cancer or genetic predispositions, regular medical check-ups and genetic counseling may help with early detection and preventive measures.
Conclusion
Pancreatic cancer is a serious and aggressive disease with a high mortality rate. However, advancements in early detection methods and treatment options offer hope for improved outcomes. Awareness of risk factors, early symptoms, and available treatments is crucial for managing pancreatic cancer. If you experience persistent symptoms such as unexplained weight loss, jaundice, or abdominal pain, it’s important to seek medical evaluation promptly for early diagnosis and treatment.
Related Videos
Discover more from CancerSurgery
Subscribe to get the latest posts sent to your email.