Rectum Cancer Treatment: Options and Considerations
Rectal cancer treatment has evolved significantly, and one of the advancements is the possibility of avoiding a permanent stoma, which can be a major concern, especially for patients with lower rectum cancer. A stoma is an opening created surgically to allow waste to exit the body when the normal route is not available. In the context of rectal cancer, a permanent stoma has traditionally been a common outcome, but advances in modern surgical techniques, better understanding of how cancer spread, and treatment strategies offer alternatives. How to avoid permanent stoma in rectum cancer treatment is one of the fundamental question asked by patients along with cure of rectum cancer.
The key to avoiding a permanent stoma lies in early detection and the precise staging of the cancer. For very early-stage, small and very superficial low rectal cancers, Transanal endoscopic microsurgery (TEM) can be done, It is a minimally invasive surgical technique performed through the anus using an endoscope and specialized instruments to remove superficial inner layers of rectum surrounding cancer while preserving the deeper muscle layer.
For more advanced cancers, a combination of radiation therapy and chemotherapy (Neoadjuvant Chemoradiotherapy) are administered before surgery to shrink the tumor, which may sometimes allow for sphincter-preserving surgeries. These procedures aim to remove the cancer while maintaining the normal function of the rectum and anus. For these patients with low rectal tumors, a coloanal anastomosis is done. This procedure involves connecting the colon directly to the anus after the cancerous portion of the rectum has been removed. The success of this surgery depends on achieving a safe margin of cancer-free tissue and ensuring a good blood supply to the remaining bowel.
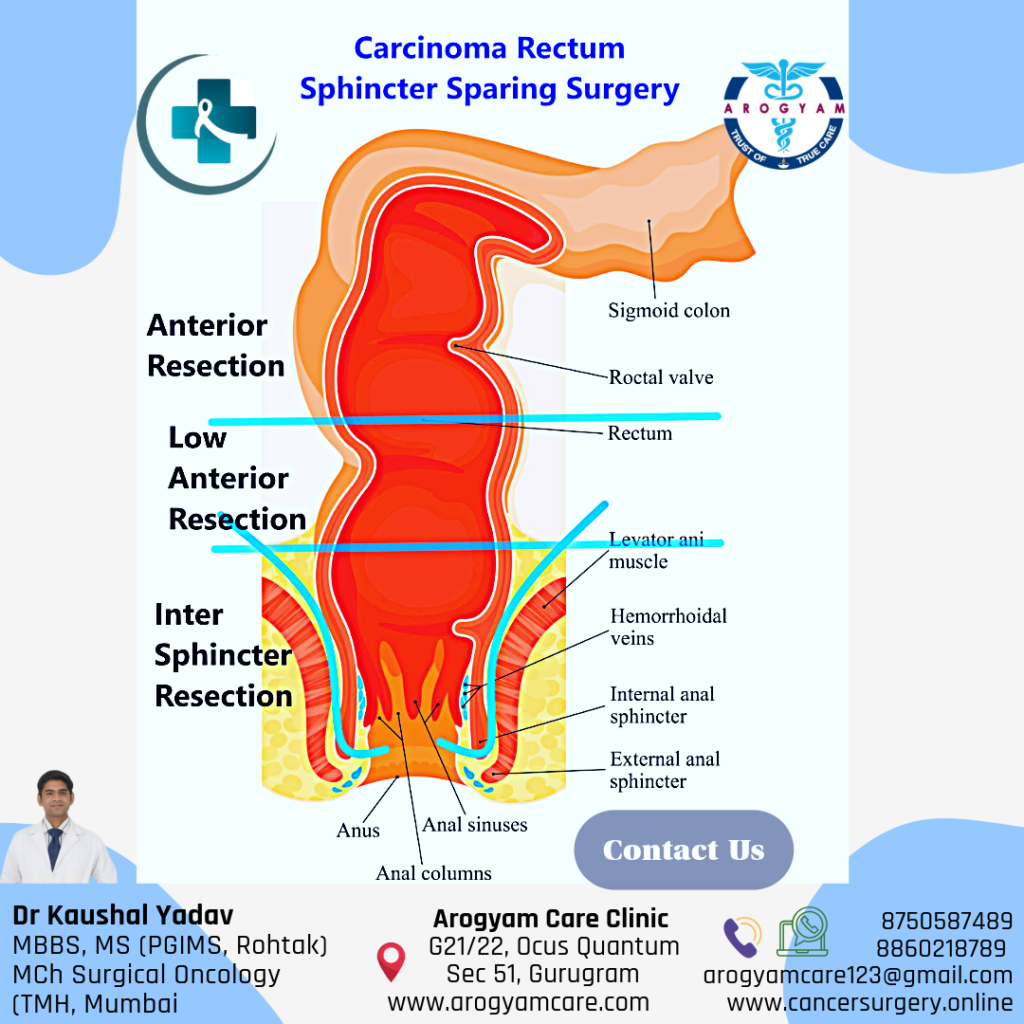
Commonly performed Sphincter preserving surgical approaches for low rectum cancer by best colorectal cancer surgeon includes:
1. Low Anterior Resection (LAR):
The cancer bearing Segment of rectum with adequate margin of normal tissue around the cancer is removed, along with nearby lymph nodes and other tissues around the rectum. The colon is then reattached to the remaining rectum maintaining normal bowel function.
2. Ultralow Anterior Resection (ULAR):
remove the cancer in lower rectum while preserving the anal sphincter. The proximal colon is then reconnected to the anal canal, maintaining normal bowel function.
3.Intersphicteric resection (ISR):
In case of very low lying cancer where external anal sphincter (Levator ani muscle) is safe from disease and has adequate tone and normal margin can be taken distally. Proximal colon is anastomosed to anal canal.
Short-term temporary stoma may be made in case of frail patients or difficult anastomosis. The end of the intestine is brought out through a hole in the skin of the abdomen. This gives the rectum time to heal before stool moves through it. Mostly stoma is reversed (the intestines reconnected) after adequate healing.
The decision-making process for rectal cancer surgery is complex and highly individualized. Factors such as the tumor’s location, size, and the patient’s overall health and preferences play a crucial role. Surgeons aim to perform a high-quality cancer operation while preserving the patient’s quality of life, which includes avoiding a permanent stoma whenever possible. These surgeries can be done by open, laparoscopic or robotic approaches by equally good success
While a permanent stoma was once a common result of rectal cancer surgery, advancements in surgical techniques have made it possible to avoid it in many cases. Patients should engage in open dialogue with their Oncosurgeon to understand their options and make informed decisions about their treatment plans.
Treatment Options for Rectal Cancer
Treatment for rectal cancer often involves a combination of therapies designed to remove the cancer, prevent its spread, and reduce the risk of recurrence. The main treatment options include:
-
Surgery
- Local Excision: If the cancer is detected early and is small, it may be removed through local excision, where the tumor and some surrounding tissue are removed without major surgery.
- Low Anterior Resection (LAR): For cancers in the upper part of the rectum, LAR involves removing the cancerous portion of the rectum and reconnecting the colon to the remaining rectum.
- Abdominoperineal Resection (APR): In cases where the cancer is lower in the rectum, close to the anus, APR may be necessary. This procedure involves removing the entire rectum and anus, requiring the creation of a permanent colostomy, where waste exits the body through an opening in the abdomen.
- Total Mesorectal Excision (TME): This surgery is often performed for mid to low rectal cancers and involves removing the rectum along with surrounding lymph nodes and tissues to ensure all cancerous cells are removed.
-
Radiation Therapy
- Preoperative Radiation: Radiation therapy is often used before surgery (neoadjuvant therapy) to shrink the tumor, making it easier to remove and reducing the risk of recurrence.
- Postoperative Radiation: After surgery, radiation therapy can be used to target any remaining cancer cells and reduce the risk of the cancer returning.
- External Beam Radiation: The most common type, where high-energy beams are directed at the tumor from outside the body.
-
Chemotherapy
- Neoadjuvant Chemotherapy: Often combined with radiation therapy before surgery to shrink the tumor and make surgery more effective.
- Adjuvant Chemotherapy: Given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Chemoradiation: A combination of chemotherapy and radiation therapy, used together to enhance the effectiveness of both treatments.
-
Targeted Therapy
- Targeted therapy involves using drugs that specifically target the cancer cells, often with fewer side effects than traditional chemotherapy. These drugs can block the growth of cancer cells by interfering with specific molecules involved in tumor growth and progression.
- Commonly used targeted therapies for rectal cancer include Bevacizumab (Avastin) and Cetuximab (Erbitux).
-
Immunotherapy
- Immunotherapy uses the body’s immune system to fight cancer. This approach is particularly effective for certain types of rectal cancer that have specific genetic markers, such as microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR).
- Drugs like Pembrolizumab (Keytruda) and Nivolumab (Opdivo) are examples of immunotherapies that may be used in these cases.
-
Palliative Care
- For advanced stages of rectal cancer where the goal is to manage symptoms and improve quality of life rather than cure the disease, palliative care becomes an important aspect of treatment. This may include pain management, nutrition support, and psychological counseling.
Factors Influencing Treatment Decisions
Choosing the right treatment for rectal cancer depends on several key factors:
- Stage of Cancer: Early-stage rectal cancer may be treated with surgery alone, while more advanced stages often require a combination of treatments.
- Location of the Tumor: The exact location of the tumor in the rectum influences the type of surgery required and whether a colostomy will be necessary.
- Patient’s Overall Health: The patient’s ability to tolerate certain treatments, such as surgery or chemotherapy, plays a crucial role in determining the best approach.
- Patient Preferences: The patient’s personal preferences regarding quality of life, potential side effects, and the desire to preserve normal bowel function are important considerations in the treatment plan.
Post-Treatment Care and Follow-Up
After treatment for rectal cancer, ongoing care is essential to monitor for any signs of recurrence and manage any long-term side effects. This may include:
- Regular Follow-Up Visits: These may involve physical exams, blood tests, imaging tests, and colonoscopies to check for signs of cancer recurrence.
- Lifestyle Changes: Maintaining a healthy diet, exercising regularly, and avoiding tobacco and excessive alcohol can help reduce the risk of recurrence.
- Managing Side Effects: Post-treatment care may also involve managing side effects from surgery, radiation, or chemotherapy, such as bowel dysfunction, fatigue, or neuropathy.
To Know More About Rectum Cancer
Discover more from CancerSurgery
Subscribe to get the latest posts sent to your email.