Rectal cancer treatment has evolved significantly, and one of the advancements is the possibility of avoiding a permanent stoma, which can be a major concern, especially for patients with lower rectum cancer. A stoma is an opening created surgically to allow waste to exit the body when the normal route is not available. In the context of rectal cancer, a permanent stoma has traditionally been a common outcome, but advances in modern surgical techniques, better understanding of how cancer spread, and treatment strategies offer alternatives. How to avoid permanent stoma in rectum cancer treatment is one of the fundamental question asked by patients along with cure of rectum cancer.
The key to avoiding a permanent stoma lies in early detection and the precise staging of the cancer. For very early-stage, small and very superficial low rectal cancers, Transanal endoscopic microsurgery (TEM) can be done, It is a minimally invasive surgical technique performed through the anus using an endoscope and specialized instruments to remove superficial inner layers of rectum surrounding cancer while preserving the deeper muscle layer.
For more advanced cancers, a combination of radiation therapy and chemotherapy (Neoadjuvant Chemoradiotherapy) are administered before surgery to shrink the tumor, which may sometimes allow for sphincter-preserving surgeries. These procedures aim to remove the cancer while maintaining the normal function of the rectum and anus. For these patients with low rectal tumors, a coloanal anastomosis is done. This procedure involves connecting the colon directly to the anus after the cancerous portion of the rectum has been removed. The success of this surgery depends on achieving a safe margin of cancer-free tissue and ensuring a good blood supply to the remaining bowel.
Commonly performed Sphincter preserving surgical approaches for low rectum cancer by best colorectal cancer surgeon includes:
1. Low Anterior Resection (LAR):
The cancer bearing Segment of rectum with adequate margin of normal tissue around the cancer is removed, along with nearby lymph nodes and other tissues around the rectum. The colon is then reattached to the remaining rectum maintaining normal bowel function.
2. Ultralow Anterior Resection (ULAR):
remove the cancer in lower rectum while preserving the anal sphincter. The proximal colon is then reconnected to the anal canal, maintaining normal bowel function.
3.Intersphicteric resection (ISR):
In case of very low lying cancer where external anal sphincter (Levator ani muscle) is safe from disease and has adequate tone and normal margin can be taken distally. Proximal colon is anastomosed to anal canal. 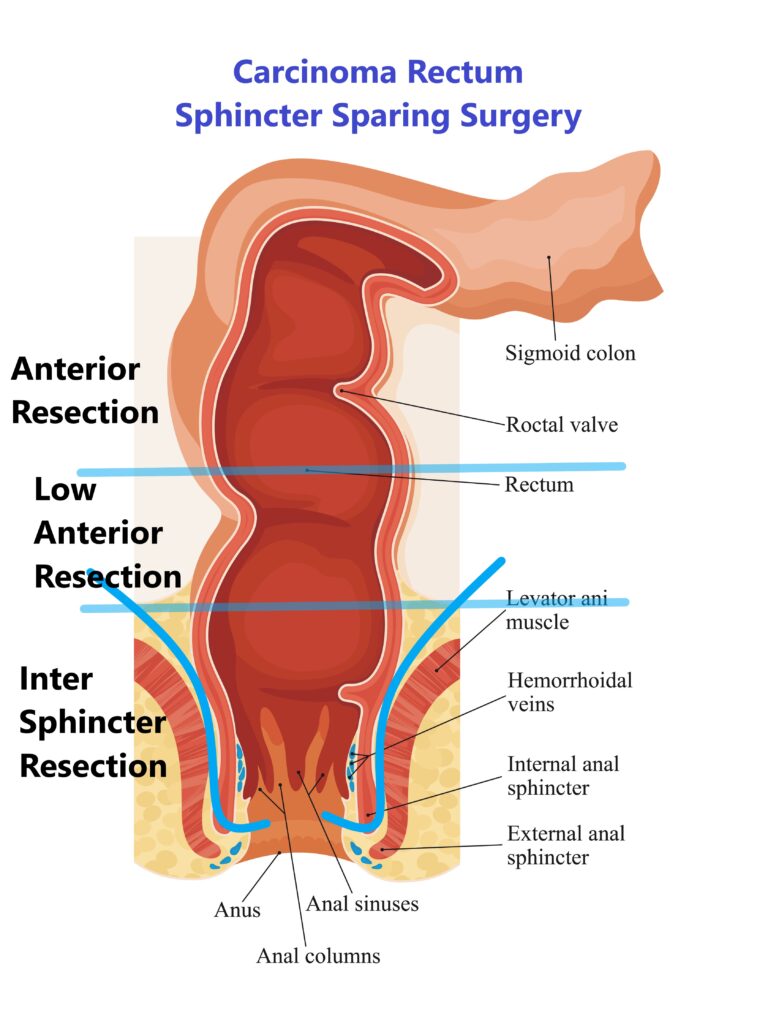
Short-term temporary stoma may be made in case of frail patients or difficult anastomosis. The end of the intestine is brought out through a hole in the skin of the abdomen. This gives the rectum time to heal before stool moves through it. Mostly stoma is reversed (the intestines reconnected) after adequate healing.
The decision-making process for rectal cancer surgery is complex and highly individualized. Factors such as the tumor’s location, size, and the patient’s overall health and preferences play a crucial role. Surgeons aim to perform a high-quality cancer operation while preserving the patient’s quality of life, which includes avoiding a permanent stoma whenever possible. These surgeries can be done by open, laparoscopic or robotic approaches by equally good success
While a permanent stoma was once a common result of rectal cancer surgery, advancements in surgical techniques have made it possible to avoid it in many cases. Patients should engage in open dialogue with their Oncosurgeon to understand their options and make informed decisions about their treatment plans.